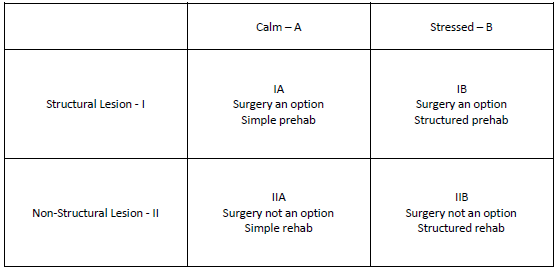
Two factors define the basic nature of your particular spine problem and determine the treatment approach.
One is the anatomy. Is there a clearly identifiable source of your pain with corresponding symptoms (structural) or is the origin unclear (non-structural)?
The second is the state of your nervous system. Are you calm and dealing well with your usual life stresses or are you feeling overwhelmed? If you are feeling stressed for more than three months, your body’s neurochemistry is on “high alert” and your immune system is creating inflammation. Every cell in your body is affected, including the speed of your nerve conduction causing more pain. Your brain becomes inflamed and sensitized to all sensory input. [1] You will not only experience more pain, your capacity to cope with it is compromised.
Your situation will fall into one of four categories:
- IA—Structural lesion, calm
- IB—Structural lesion, stressed
- IIA—Non-structural lesion, calm
- IIB—Non-structural lesion, stressed
An overview of how this looks is presented in this grid:
Type I
The implications of this grid are important in making your decisions. It will be the basis of the discussions regarding the role of surgery in your care. I have found out that if a patient is not under a lot of stress then outcomes are consistently positive if a structural problem is surgically addressed (IA). However, if that same person is in the middle of a major personal or professional crisis, then the results are less predictable (IB). Surgery may still be helpful but other factors need to be addressed.
Type II
Patients who aren’t under a lot of extra stress and are experiencing pain without a clear source (Type IIA) simply do not want or request surgery. Why? It is just pain that they can tolerate until it resolves, and it usually does.
The biggest problem we have in spine surgery is performing surgery on people who are stressed and the source of pain can’t be identified (IIB). Since mental and physical pain are processed in a similar area of the brain with the same chemical response of adrenaline and cortisol, the pain is often intense and people become desperate. There is damaging concept that is often mentioned is that since everything else has been tried, let’s do surgery. That does not make any sense in that you cannot fix what you cannot see!
Don’t become a failed spine surgery patient
First of all, surgery is never indicated without identifying the exact cause of symptoms. So the chances of success are already low. Then you add in the other factors that have been shown to adversely affect surgical outcomes (inadequate restful sleep, anxiety, depression, fear avoidance, poor physical conditioning, smoking, duration of pain, younger age), the chances of an operation being helpful are not only low, patients often get worse. [2] It is surgery being performed in this group that is creating a lot of ongoing pain and disability. It is tragic that pain in this group is so consistently solvable and surgery often makes it worse. Instead of solving chronic pain, modern medicine is creating it. Then when you have a bad surgical outcome, who is going to take care of you?
Do You Really Need Spine Surgery? Take Control with a Surgeon’s Advice provides the information you need to have productive conversations with your doctor in order to understand which quadrant of the Surgical Treatment Grid that you belong in and then pursue an appropriate course of action. The vast majority of chronic spine problems are solvable with or without surgery.
References
- Chen, X et al. “Stress enhances muscle nociceptor activity in the rat.” Neuroscience (2011); 185: 166 – 173.
- Perkins, FM and H Kehlet. “Chronic pain as an outcome of surgery: A Review of Predictive Factors.” Anesthesiology (2000); 93: 1123 – 1133