What is a laminae?
The spinal column consists of vertebra and disc as the front part of the spine, the spinal canal which contains the dural sac filled with fluid surrounding the spinal cord and nerves and the back part of the spine called the facet joints and laminae. The main support of the spine is the vertebra and discs. The back part provides a shingled bony roof. The joints between the laminae are called facet joints, which also provide stability to the spinal column.
What is Laminectomy and Laminotomy?
If the pressure on your spinal canal arises from the back part of the spine, the middle part of the laminae can be removed to alleviate the pressure. This procedure leaves the spinal canal open. A laminotomy is a procedure where smaller parts of the laminae are removed on one or both sides creating small holes between the laminae. It is the surgeon’s choice usually during surgery whether it is safe and effective to perform the smaller laminotomy or whether a laminectomy is required.
What conditions are treated by a Laminectomy/ laminotomy?
The most common reason for a laminectomy/ laminotomy is spinal stenosis. This condition occurs over time. In some people with age the ligaments between the laminae thicken and the facets enlarge. Often discrete bone spurs will form pinching a nerve. A person can also be born with a small spinal canal called a congenital spinal stenosis. Less common conditions requiring decompression include a facet cyst, fracture, and tumors.
What is believed to be the cause for spinal stenosis?
It is unclear why some people have spinal stenosis and other do not. It is felt to be due to repeated stresses over time. As the above mentioned structures thicken the space for the nerves become smaller. The appearance is similar to that of an hour glass. Symptoms won’t appear until a threshold amount of constriction occurs.
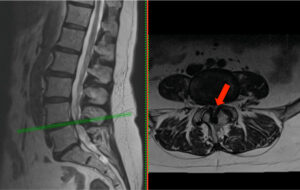
Spinal stenosis is a common problem in people over fifty years old. It is most common between the third and fourth, and the fourth and fifth lumbar vertebrae and is more common in women.
The pressure on these nerves increase when you are standing or walking, causing an increase in your back pain and your leg pain. The leg symptoms are quite varied, ranging from mild aching to severe fatigue. Leg pain, buttocks pain, pins-and-needles sensations, numbness and multiple combinations of these symptoms are also common. Often your ability to walk is limited to a few blocks or less.
The goal of a laminectomy or laminotomy is to enlarge the openings for your nerves by removing the excess bone and soft tissue. Enough of these offending structures are removed to free the nerves, but not so much that the spine is rendered unstable.
What is involved with the surgery?
An incision is made in your back or in some situations a tube retractor may be inserted. Once the laminae have been exposed a microscope is usually used to improve the safety by better visualization. As little bone removed as possible to minimize the effect on the spinal column. The surgery takes approximately an hour per level depending on the severity of the stenosis. You will be asked to get out of bed the next day after the surgery. IV pain medications are aggressively used to minimize discomfort. It is much safer to mobilize as quickly as possible. A common problem is that your bladder may not function properly due to pain medication and anesthesia. This may require a catheter for 1-2 days. It is also common to have some post-op nausea and occasional vomiting. You will be discharged home when you are mobile, eating, off IV pain medication and your bladder is functioning.
What symptoms are relieved with a laminectomy or laminotomy?
The symptoms in your buttocks and legs are the ones most reliably relieved with this surgery. These symptoms include numbness, tingling, aching, heaviness, weakness, and inability to walk. If your leg symptoms are made worse with sitting rather than standing or walking the diagnosis of spinal stenosis should be in question. This operation does not reliably relieve low back pain. If you have only low back pain and no leg symptoms you should probably not undergo this surgery.
If you have leg weakness before the surgery the strength is unlikely to return. Resolution of numbness is unpredictable.
What is the over all success rate?
The success will depend on your specific pathology. However the success rate is around 65-70%. This does not mean symptom free. Usually there is residual backache or some leg symptoms, which are an annoyance. You should have an improved ability to walk. As you probably have not vigorously walked for a while before the surgery it may take months to rebuild the muscle strength. Around 30% of patients don’t improve to their satisfaction and there is a chance that you could be made worse if the nervous system is not calmed down first.
What can I do when I go home?
As we are removing just enough bone and ligaments to decompress the nerve your spine is considered stable immediately. The healing that takes place is the muscles, skin and the nerves adapting to having the pressure removed. You can be as active as your pain allows. You can ride in a car, climb stairs, and generally perform your normal activities. Generally we like you to wait around 6 weeks prior to engaging in more vigorous exercise.
What are the most significant risks of the surgery?
Inadequate Pain Relief
If your nerves are permanently damaged or not enough pressure is removed from the nerves you will have ongoing leg symptoms. Even the most successful operation often has some mild residual numbness, tingling or pain. As mentioned earlier this operation does not reliably relieve back pain. If too much bone is removed or your bone is too soft your spine may become unstable causing increased back pain. This situation may require a fusion to stabilize the spine. As the muscles of your back are disrupted it is common for even successful operations to have a mild low back pain.
Infection
The risk of deep infections is around 1-2%. This usually occurs 1-2 weeks after surgery and is manifested by wound drainage. Further surgery is required to clean the infection followed by 6 weeks of IV antibiotics. There may be a mild superficial wound infection, which easily resolves within 1-2 weeks with oral antibiotics.
Dural Tear
Around 5-10% of the time the sac of fluid enclosing your nerve is inadvertently entered. Most of the time these are easily repaired. However you would be required to stay flat in bed for 3 days to allow the leak to seal. Occasionally this leak does not seal which may require a diverting drain or a second operation.
Nerve Damage
If you already have weak muscles in your legs from damaged nerves it is rare to have the weakness resolve. There is a small chance during surgery the nerves to your legs could be damaged. This may result in weakness in one or several parts of your leg. It does not generally result in paraplegia but occasionally the weakness may be quite significant. This is due to the fact the compressing tissues can be very adherent to the nerves. This damage may or may not resolve. Very rarely serious loss can occur such as loss of bowel and bladder functions and can be permanent.
Blood Clots
As you have been less active due to your pain there is a risk of blood clots forming in our legs. These can break off and travel to your lungs, which is called a pulmonary embolism. Occasionally this can be a fatal event.
Medical Complications
Medical complications may occur with any surgery. Your general health is the risk factor. It has been found that age in and of itself is not a risk factor. These complications include heart attack, stroke, respiratory failure or rarely death. These severe complications are less common than with more major surgeries such as fusion.
Minor Complications
Events such as bladder infections, pneumonia, ileus (stomach not passing through food), fever, inability to urinate, sore throat, and medication reactions are usually short lived but may prolong hospital stay. You may have headaches due to medications and anesthesia. There may be unanticipated complications.
Overview
If your symptoms in your legs are just annoying and mild you probably should not undergo the operation. However if your quality of life is significantly improved the surgery can be very beneficial. This is most of the time considered elective surgery so it is your responsibility to determine if your symptoms warrant the risk of surgery. There is often a fear that the surgery is not done you will be paralyzed and end up in a wheelchair. This is essentially unheard of and should not be the factor in deciding whether to proceed with surgery.
Please ask any and all questions, as this is an important decision.