Please do not let this happen to you, your family, or friends. The downside of failed spine surgery can be catastrophic, and it is impossible for you, as a patient, to comprehend how bad it can be. Complications happen with every surgeon, including me. That is not the issue. The main question is, “was surgery necessary in the first place?” If not, then this situation is even more of a tragedy. The second question is, “if so, was everything possible done before surgery to optimize the chances of success?” As bad as this patient’s story is, it is not an uncommon occurrence. This email was sent into my website, and I don’t any more details than what you are reading.
A patient’s story – spine surgery gone bad
I had anterior/posterior surgery on election day 2008. I was taken directly to the furthest room from the nurse’s station with no monitors. My husband came in to visit me and I was not breathing. As he called out…I had an out of body experience watching the doctor enter the room and watched him yelling for nurses. They put me into ICU for 4 days.
A number of things happened including the doctor ignoring me when I told him of things I felt were wrong. When they sent me to rehab, they sent me sitting up in a wheelchair van. PAINFUL. I was an inpatient for three days. The 2nd day home I was sent to ER with MRSA, sepsis and three blood clots. In total, I was in hospitals for 2 months.
The end results were that I couldn’t sit for any length of time without pain forcing me to retire on disability….sex was and still is impossible. Even a slight jolt shoots pain through my back. Cannot motorcycle any longer. Can’t walk on uneven surfaces like beaches. Can’t walk long distances. And am permanently on 2 pain meds to be functional without pain. My whole life changed in many ways as a result of this surgery directly and indirectly. At one point they dropped me…hitting the NG tube and knocking it out. That damaged the interior of my nose, and it has never been the same.
I wish I’d never had it. But because I couldn’t walk for more than 3 days before I was in bed with debilitating pain, I didn’t feel I had a choice. I was fused from L2 to S1 (bottom four levels of the lumbar spine).

My perspective
I am going simply list the issues in this situation.
- This surgery was probably performed for degenerative disc disease and back pain. Disc degeneration is not a disease, is part of the normal aging process, and has been well documented to NOT be a source of pain.1
- The success rate of a spine fusion (welding vertebrae together with metal and bone) for back pain is < 30%.2 There is not one research paper that has ever shown that a lumbar fusion for chronic LBP is effective compared with thoughtfully implemented rehab.
- The data also shows that when you have an operation in the presence of untreated chronic pain, you can induce chronic pain at the surgical site (or make it worse) between 40-60% of the time.3 In other words, there is almost double the chance of making a patient worse than solving the problem.
- There is little attention paid to optimizing the chances of success of an elective spine surgery. One paper showed that only 10% of surgeons addressed the known risk factors for poor outcomes prior to surgery.4
- For example, lack of sleep has been shown to CAUSE chronic low back pain. How many surgeons are attending to just that one detail prior to recommending surgery?5
- The more levels of the spine that are fused, the higher the complication rate. This person had four levels fused and was fused both through the front and back of the spine. This is a big operation.
- People will undergo surgery because “everything else has been done.” That is simply not true. By systematically addressing all of the factors that affect the complexity of chronic pain, it is a consistently solvable problem.
- 90% of all chronic mental and physical symptoms in your body are physiological and created by sustained exposure to flight or fight stress chemistry. When your body stays revved up, it will predictably break down. The solution lies in learning ways to regulate your threat physiology to that of safety.
- Many surgical decisions are made quickly on the first visit and sometimes you may not even meet the surgeon. This makes no sense. Chronic pain is complex, you are unique, it impossible to deeply understand a situation in any domain of life on one visit.
- We put all of our patients through a minimum of 12 weeks rehab before any elective surgery, and longer if the variables affecting pain weren’t successfully addressed. The process was called, “prehab.”
Do You Really Need Spine Surgery?
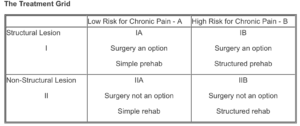
I could write a book on this situation, and I did. It is Do You Really Need Spine Surgery? Take Control with a Surgeon’s Advice.6 It breaks down the decision-making around spine surgery into two factors.
- The nature of the anatomy
- The state of the nervous system
You’ll fall into one of four quadrants and the choices are clear. If you have a specific anatomical problem with matching symptoms and your nervous system is calm, surgical outcomes are much more predictable. Every other situation is problematic but still solvable.
I am not just trying to sell a book today. My mission is to do what I can do to slow down the juggernaut of aggressive spine surgery.
I was a surgeon who was called a “salvage surgeon.” I would see patients that had many surgeries over their lifetime, and their lives were destroyed. I was able to help many of them out, but it was more with the rehab than with the additional surgeries. At the same time, I was seeing so many patients break free from the grip chronic mental and physical pain with the concepts presented in The DOC Journey, that I could no longer just sit on the sidelines. There were minimal costs, no risks, and patients would thrive. All of the treatments are based on effective and deeply documented modalities.
Be careful
Please do not jump into any spine surgery without really understanding the issues and maximizing your chances of success. Certainly, do not allow any decisions of this magnitude to be made on the first visit. This person had better choices, but they were not presented or implemented.
Chronic pain is a solvable problem, with or without surgery. Surgery is only an option if there is a surgical lesion. A normally aging spine is not in this category. Do not become one of the patients in this blog who has had their life destroyed. As bad as your chronic pain is at the moment, it can be made a lot worse with an ill-advised operation. It is even more tragic in that the solution, as many of my patients have said is, “disturbingly simple.” Do not just trust a physician you barely know. The basic step is to develop a relationship with him or her. Then take control of your decision, pain, and life.
There is still hope
I don’t want this article to end on a down note. As bad as this situation looks, it is still a solvable issue. Your brain is incredibly adaptable, and you can reprogram it in any direction you choose. I have seen many patients in this bad of shape eventually become free of pain. One gentleman had undergone 28 surgeries in 22 years and has now been free of pain for over six years. In fact, he says that “I have never felt better in my life.” Another woman had been in pain for 50 years and has done well for over seven years.
The main factor that determines success is simply your willingness to engage or as one my successful patients has said, “suspend your disbelief.”
Please share your story of a failed spine surgery. I am more than aware that there are many successes, even for chronic low back pain. It is just that the success rate is not high enough to justify the risks of surgery and there are alternatives that are so much better. The world needs to know the downside of a failed spine operation in order to make more informed decision.
References
- Jensen MC, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. NEJM (1994); 331:69-73
- Carragee EJ et al. A Gold Standard Evaluation of the ‘Discogenic Pain’ Diagnosis as Determined by Provocative Discography. Spine (2006) 31: 2115 – 2123.
- Perkins FM and H Kehlet. Chronic pain as an outcome of surgery: A Review of Predictive Factors. Anesthesiology (2000); 93:1123–1133.
- Young AK, et al. “Assessment of presurgical psychological screening in patients undergoing spine surgery.” Journal Spinal Disorders Tech (2014); 27: 76-79.
- Agmon M and Galit Armon. “Increased insomnia symptoms predict the onset of back pain among employed adults.” PLOS One (2014); 9: 1-7.
- Hanscom David. Do You Really Need Spine Surgery? Take Control with a Spine Surgeon’s Advice. Vertus Press, Oakland, CA, 2019.
