I am a busy spine surgeon, yet I spend most of my time talking my patients out of surgery. When I do recommend surgical treatment, many, if not most, become apprehensive. They have heard that spine surgery never works and will relate stories to me about their friends, family, or co-workers who have had a poor outcome. My response is that spine surgery does have a bad reputation, and unfortunately it is well deserved.
As you age, the discs between your vertebrae lose water content and become stiffer. That is a normal part aging. You lose flexibility. Over age 50 most people have degeneration of at least one disc. There is no evidence that supports the idea that a degenerated disc causes pain. (1)
At age 32, I underwent a disc excision for a ruptured disc followed by a second operation two weeks later for a deep wound infection. My three lowest discs are completely degenerated and collapsed. Other than an occasional muscle strain from my terrible golf swing, I do not experience back pain. I saw patients weekly with “terrible looking spines” and sciatica from pinched nerves. However, most of them had no back pain. The upshot is that most spine fusions for LBP are performed on normal spines for a given person’s age. The results are poor. There is less than a 30% chance of long-term success. (2)
If there is an identifiable structural problem with a matching pattern of pain, the success rate of surgery is much higher. These are the only situations that I will perform surgery. An example would be a bone spur pinching the 5th lumbar nerve root while there is pain down the side of the patient’s leg. In this case, there is a strong correlation between the structural description and the pain. This pattern of pain usually disappears after surgically removing the spur.
Mouth pain vs. a cavity
I frequently compare spine surgery with dentistry. Generally a dentist can specifically identify the structural problem causing your pain. It might be a cavity that has gone down to the root. The chance that your dentist can solve this problem with a filling, root canal, crown, etc. is essentially 100%.
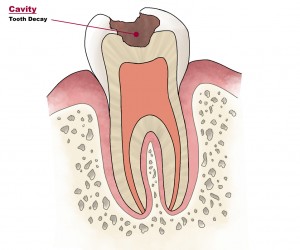
What if you went to your dentist with “mouth pain,” but the source of the pain could not be identified? This is also a common occurrence. The pain may emanate from the sinuses, be caused by TMJ, or can even be a “neurophysiological” symptom. What would be the chance of success if your dentist started doing procedures without seeing which tooth was the source of the pain? It would be almost zero.
Fusions for back pain
Currently there are hundreds of thousands of spine fusions being performed annually for “back pain.” Often, they are based on injections into the discs called discograms that have been shown to be unreliable. Or they are based on MRI’s showing “degenerative changes.” We know bone spurs, arthritis, and degenerated discs do not correlate well with back pain. Yet major structural bony interventions are being performed with the surgical world not being able to accurately diagnose the source of the pain. Many surgeons feel somewhat compelled to perform the surgery because it is the “last resort.”
Fusions not only are ineffective in relieving back pain, but the downside risk of complications and breakdown of the spine often creates serious problems. There is even a medical term called “Failed Back Syndrome”. What is not well-known is the extent of the destruction caused on these patients’ lives. I discuss this outcome in the appendix of my books, Back in Control and in Do You Really Need Spine Surgery? Take Control with a Spine Surgeon’s Advice. Many of these situations were catastrophic.
Surgery is not the “definitive” answer for lower back pain. It is usually the wrong answer!!!
- Boden, SD et al. “Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: A prospective investigation.” Journal of Bone and Joint Surgery(1990); 72: 403 – 8.
- Carragee, EJ et al. “A Gold Standard Evaluation of the ‘Discogenic Pain’ Diagnosis as Determined by Provocative Discography.”Spine(2006) 31: 2115 – 2123.
